Home > about eyes > Cataracts
Cataracts
Cataracts
Cataracts are the leading cause of blindness in the world today (especially in countries where access to surgical procedures are lacking), and are one of the leading causes of impaired vision in New Zealand, with a large percentage of the elderly population exhibiting some signs of the condition. In 2005, the Government in this country pledged to spend an extra $17 million over the next three years in providing a total of up to 7500 more cataracts operations. The NZ Ministry of Health said that by 2007-08 they hoped to be performing more than 12,000 operations a year, a 50 percent increase on 2005.
 |
 |
What is a cataract?
|
 |
The lens
|
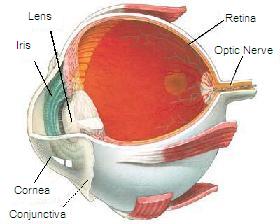
The lens is a clear part of the eye that helps to focus light, or an image, on the retina. The retina is the light-sensitive tissue at the back of the eye. In a normal eye, light passes through the transparent lens to the retina. Once it reaches the retina, light is changed into nerve signals that are sent to the brain. The lens must be clear for the retina to receive a sharp image. If the lens is milky or cloudy from a cataract, the image you see will be blurred. |
|
Other types of cataract
Yes. Although most cataracts are related to aging (Senile cataracts), there are other types of cataract:
- Secondary cataract. Cataracts can form after surgery for other eye problems, such as glaucoma. Cataracts also can develop in people who have other health problems, such as diabetes. Cataracts are sometimes linked to steroid use.
- Traumatic cataract. Cataracts can develop after an eye injury, sometimes years later.
- Congenital cataract. Some babies are born with cataracts or develop them in childhood, often in both eyes. These cataracts may be so small that they do not affect vision. If they do, the lenses may need to be removed.
- Radiation cataract. Cataracts can develop after exposure to some types of radiation.
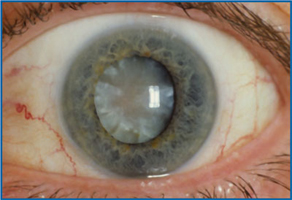
A senile cataract, occurring in the elderly, is characterized by an initial opacity in the lens, subsequent swelling of the lens and final shrinkage with complete loss of transparency. Moreover, with time the cataract cortex liquefies to form a milky white fluid in a Morgagnian cataract, which can cause severe inflammation if the lens capsule ruptures and leaks. Untreated, the cataract can cause phacomorphic glaucoma. Very advanced cataracts with weak zonules are liable to dislocation anteriorly or posteriorly. Such spontaneous posterior dislocations (akin to the historical surgical procedure of couching) in ancient times were regarded as a blessing from the heavens, because some perception of light was restored in the cataractous patients
Treatment
The symptoms of early cataract may be improved with new eyeglasses, brighter lighting, anti-glare sunglasses, or magnifying lenses. If these measures do not help, surgery is the only effective treatment. Surgery involves removing the cloudy lens and replacing it with an artificial lens.
|
A cataract needs to be removed only when vision loss interferes with your everyday activities, such as driving, reading, or watching TV. See our optometrist for further advice. Once you understand the benefits and risks of surgery, you can make an informed decision about whether cataract surgery is right for you. In most cases, delaying cataract surgery will not cause long-term damage to your eye or make the surgery more difficult. You do not have to rush into surgery. |
 |
Sometimes a cataract should be removed even if it does not cause problems with your vision. For example, a cataract should be removed if it prevents examination or treatment of another eye problem, such as age-related macular degeneration or diabetic retinopathy. If your eye care professional finds a cataract, you may not need cataract surgery for several years. In fact, you might never need cataract surgery. By having your vision tested regularly, you and your eye care professional can discuss if and when you might need treatment.
If you have cataracts in both eyes that require surgery, the surgery will be performed on each eye at separate times, usually four to eight weeks apart.
What are the different types of cataract surgery?
 |
There are two types of cataract surgery:
|
After the natural lens has been removed, it often is replaced by an artificial lens, called an intraocular lens (IOL). An IOL is a clear, plastic lens that requires no care and becomes a permanent part of your eye. Light is focused clearly by the IOL onto the retina, improving your vision. You will not feel or see the new lens. Some people cannot have an IOL. They may have another eye disease or have problems during surgery. For these patients, a soft contact lens, or glasses that provide high magnification, may be suggested.
What are the risks of cataract surgery?
As with any surgery, cataract surgery poses risks, such as infection and bleeding. Before cataract surgery, your doctor may ask you to temporarily stop taking certain medications that increase the risk of bleeding during surgery. After surgery, you must keep your eye clean, wash your hands before touching your eye, and use the prescribed medications to help minimize the risk of infection. Serious infection can result in loss of vision.
Cataract surgery slightly increases your risk of retinal detachment. Other eye disorders, such as high myopia (nearsightedness), can further increase your risk of retinal detachment after cataract surgery. One sign of a retinal detachment is a sudden increase in flashes or floaters. Floaters are little "cobwebs" or specks that seem to float about in your field of vision. If you notice a sudden increase in floaters or flashes, see an eye care professional immediately. A retinal detachment is a medical emergency. If necessary, go to an emergency service or hospital. Your eye must be examined by an eye surgeon as soon as possible. A retinal detachment causes no pain. Early treatment for retinal detachment often can prevent permanent loss of vision. The sooner you get treatment, the more likely you will regain good vision. Even if you are treated promptly, some vision may be lost.
Is cataract surgery effective?
Cataract removal is a very common operation. It also is one of the safest and most effective types of surgery. In about 90 percent of cases, people who have cataract surgery have better vision afterward.
What happens before surgery?
A week or two before surgery, your opthalmologist will do some tests. These tests may include measuring the curve of the cornea and the size and shape of your eye. This information helps your doctor choose the right type of IOL.
You may be asked not to eat or drink anything 12 hours before your surgery.
What happens during surgery?
At the hospital or eye clinic, drops will be put into your eye to dilate the pupil. The area around your eye will be washed and cleansed.
The operation usually lasts less than one hour and is almost painless. Many people choose to stay awake during surgery. Others may need to be put to sleep for a short time.
If you are awake, you will have an anesthetic to numb the nerves in and around your eye.
After the operation, a patch may be placed over your eye. You will rest for a while. Your medical team will watch for any problems, such as bleeding. Most people who have cataract surgery can go home the same day. You will need someone to drive you home.
What happens after surgery?
Itching and mild discomfort are normal after cataract surgery. Some fluid discharge is also common. Your eye may be sensitive to light and touch. If you have discomfort, your doctor can suggest treatment. After one or two days, moderate discomfort should disappear.
For a few days after surgery, your opthalmologist may ask you to use eyedrops to help healing and decrease the risk of infection. You will need to wear an eye shield or eyeglasses to help protect your eye. Avoid rubbing or pressing on your eye.
When you are home, try not to bend from the waist to pick up objects on the floor. Do not lift any heavy objects. You can walk, climb stairs, and do light household chores.
In most cases, healing will be complete within eight weeks. Your doctor will schedule exams to check on your progress.
Can problems develop after surgery?
Problems after surgery are rare, but they can occur. These problems can include infection, bleeding, inflammation (pain, redness, swelling), loss of vision, double vision, and high or low eye pressure. With prompt medical attention, these problems can usually be treated successfully.
Sometimes the eye tissue that encloses the IOL becomes cloudy and may blur your vision. This condition is called an after-cataract. An after-cataract can develop months or years after cataract surgery.
An after-cataract is treated with a laser. Your surgeon uses a laser to make a tiny hole in the eye tissue behind the lens to let light pass through. This outpatient procedure is called a YAG laser capsulotomy. It is painless and rarely results in increased eye pressure or other eye problems. As a precaution, your doctor may give you eyedrops to lower your eye pressure before or after the procedure.
For more information contact our Optometrist



