Home > about eyes > Diabetic Retinopathy
Diabetic Retinopathy
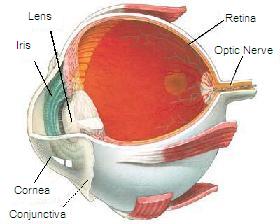
Diabetic retinopathy is damage to the eye's retina that occurs with long-term diabetes.
Causes, incidence, and risk factors
There are two types, or stages of retinopathy: Nonproliferative or proliferative
-
Nonproliferative diabetic retinopathy develops first. Blood vessels in the eye become larger in certain spots (called microaneurysms). Blood vessels may also become blocked. There may be small amounts of bleeding (retinal hemorrhages), and fluid may leak into the retina. This can lead to noticeable problems with your eyesight.
-
Proliferative retinopathy is the more advanced and severe form of the disease. New blood vessels start to grow in the eye. These new vessels are fragile and can bleed (hemorrhage). Small scars develop, both on the retina and in other parts of the eye (the vitreous). The end result is vision loss, as well as other problems.
Other problems that may develop are:
-
Macular edema -- the macula is the area of the retina that provides sharp vision straight in front of you. If fluid leaks into this area, your vision becomes more blurry.
-
Retinal detachment -- scarring may cause part of the retina to pull away from the back of your eyeball.
-
Glaucoma -- increased pressure in the eye is called glaucoma. If not treated, it can lead to blindness.
Diabetic retinopathy is a leading cause of blindness in working-age New Zealanders. People with both type 1 diabetes and type 2 diabetes are at risk for this condition.
Having more severe diabetes for a longer period of time increases the chance of getting retinopathy. Retinopathy is also more likely to occur earlier and be more severe if your diabetes has been poorly controlled. Almost everyone who has had diabetes for more than 30 years will show signs of diabetic retinopathy.
Symptoms
Most often, diabetic retinopathy has no symptoms until the damage to your eyes is severe.
Symptoms of diabetic retinopathy include:
-
Blurred vision and gradual vision loss
-
Shadows or missing areas of vision
-
Difficulty seeing at nighttime
Many people with early diabetic retinopathy have no symptoms before major bleeding occurs in the eye. This is why everyone with diabetes should have regular eye exams.
 Normal Vision |
 Simulated Diabetic Retinopathy Vision |
Signs and tests
In nearly all cases, the health care provider can diagnose diabetic retinopathy by dilating the pupils with eye drops and then carefully examining the retina. A retinal photography or fluorescein angiography test may also be used.
Treatment
The following are very important for preventing diabetic retinopathy:
-
Tight control of blood sugar (glucose), blood pressure, and cholesterol
-
Stopping smoking
People with nonproliferative diabetic retinopathy may not need treatment. However, they should be closely followed-up by an opthalmologist trained to treat diabetic retinopathy.
Treatment usually does not reverse damage that has already occurred, but it can help keep the disease from getting worse. Once your eye doctor notices new blood vessels growing in your retina (neovascularization) or you develop macular edema, treatment is usually needed.
Several procedures or surgeries are the main treatment for diabetic retinopathy.
Laser eye surgery creates small burns in the retina where there are abnormal blood vessels. This process is called photocoagulation. It is used to keep vessels from leaking or to get rid of abnormal, fragile vessels.
-
Focal laser photocoagulation is used to treat macular edema.
-
Scatter laser treatment or panretinal photocoagulation treats a large area of your retina. Often two or more sessions are needed.
A surgical procedure called vitrectomy is used when there is bleeding (hemorrhage) into the eye. It may also be used to repair retinal detachment.
Drugs that prevent abnormal blood vessels from growing, and corticosteroids injected into the eyeball are being investigated as new treatments for diabetic retinopathy.
If you cannot see well:
-
Make sure your home is safe so you do not fall
-
Organize your home so that you can easily find what you need
-
Get help to make sure you are taking your medicines correctly
Support Groups
Diabetes New Zealand - www.diabetes.org.nz
Diabetes Auckland - www.diabetesauckland.org.nz
Expectations (prognosis)
You can improve your outcome by keeping good control of your blood sugar and blood pressure.
Both treatments are effective at reducing vision loss. They do not cure diabetic retinopathy or reverse the changes that have already occurred.
Once proliferative retinopathy occurs, there is always a risk for bleeding. You will need ongoing monitoring, and you may need more treatment.
Complications
-
Blindness
Calling your health care provider
Call for an appointment if you have diabetes and you have not seen an optometrist in the past year.
Call us quickly or your doctor if any of the following symptoms are new or are becoming worse:
-
You cannot see well in dim light.
-
You have blind spots.
-
You have double vision (you see two things when there is only one).
-
Your vision is hazy or blurry and you cannot focus.
-
You have pain in one of your eyes.
-
You are having headaches.
-
You see spots floating in your eyes.
-
You cannot see things on the side of your field of vision.
-
You see shadows (where there shouldn't be shadows).
Prevention
|
Tight control of blood sugar, blood pressure, and cholesterol is very important for preventing diabetic retinopathy. Do not smoke. If you need help quitting, ask your doctor or nurse. You may not know there is any damage to your eyes until the problem is very bad. Progression is painless. Your Optometrist can catch problems early if you get regular exams. You will need to see an Optometrist who is trained to screen for diabetic retinopathy regularly.
Ask about our special rates for regular diabetic eye health checks. |
 |
Eye examinations are essential as follows by an opthalmologist skilled in the treatment of diabetic retinopathy:
-
Children older than 10 years who have had diabetes for 3 - 5 years or more
-
Adults and adolescents with type 2 diabetes soon after diagnosis
-
Adolescents and adults with type 1 diabetes within 5 years of diagnosis
-
After the first exam, most patients should have a yearly eye exam.
If you are beginning a new exercise program or are planning to get pregnant, have your eyes examined. Avoid resistance or high-impact exercises, which can strain already weakened blood vessels in the eyes.
If you are at low risk, you may need follow-up exams only every 2 - 3 years. The eye exam should include dilation to check for signs of retinal disease (retinopathy).
References
- American Diabetes Association. Standards of medical care in diabetes--2010. Diabetes Care. 2010 Jan;33 Suppl 1:S11-61.
- O'Doherty M, Dooley I, Hickey-Dwyer M. Interventions for diabetic macular oedema: a systematic review of the literature. Br J Opthalmol. 2008;92:1581-1590.
- Diabetic Retinopathy Clinical Research Network (DRCR.net), Beck RW, Edwards AR, Aiello LP, Bressler NM, Ferris F, Glassman AR, et al. Three-year follow-up of a randomized trial comparing focal/grid photocoagulation and intravitreal triamcinolone for diabetic macular edema. Arch Ophthalmol. 2009;127:245-251.